The History of the Heart Rate Monitor
Part 2 of my "Adventures in Heart Rate Monitoring." (You can find Part 1 here.) Thanks for reading and supporting my work.
Although fitness-related wearables like the Apple Watch or the FitBit are now marketed to everyone (along with the promise, of course, that the data they gather will help one “personalize” one’s health regimen), many of the features of these devices — the hardware, the algorithms — were originally developed for very specific populations. This should prompt us to ask a lot of questions, I think, about whether or not the data we glean is useful and the “insights” we’re offered applicable to our specific physiological condition.
In the case of the heart-rate monitor, the history of the technology involves diagnosing and treating patients with heart disease and other cardiovascular conditions. But there’s another thread too, one that involves designing tools to monitor the cardiovascular capacity of elite athletes in training — quite a different population and a different scope of work. But now the heart rate monitor is a standard feature on many fitness watches, with most of us being neither of these populations.
The heart-rate monitors on newer fitness watches typically use photoplethysmography — infrared sensors that detect the expansion of arteries beneath the skin of your wrist. You can sometimes see the light shining if you peek underneath them. (Fun fact: the inventor of that little green light is a furry.) These optical readers have been found to be quite accurate, but some athletes still rely on a heart rate monitors attached to a chest strap. These use electrocardiography, detecting the electrical activity of the heart (and then, using bluetooth or similar radio signals, transmit the data to a watch or other device).
There is quite a lengthy history here — no surprise, as monitoring a heartbeat has been a window into understanding health since the earliest medical practices. We can trace the reading of a pulse back thousands of years. In the Epic of Gilgamesh, for example, **Gilgamesh laments about his dead friend, “I touch his heart but it does not beat at all” — that is to say, over 2600 years ago, ancient humans understood the importance of the heart as an organ tied to life and knew that its beating could be palpated.
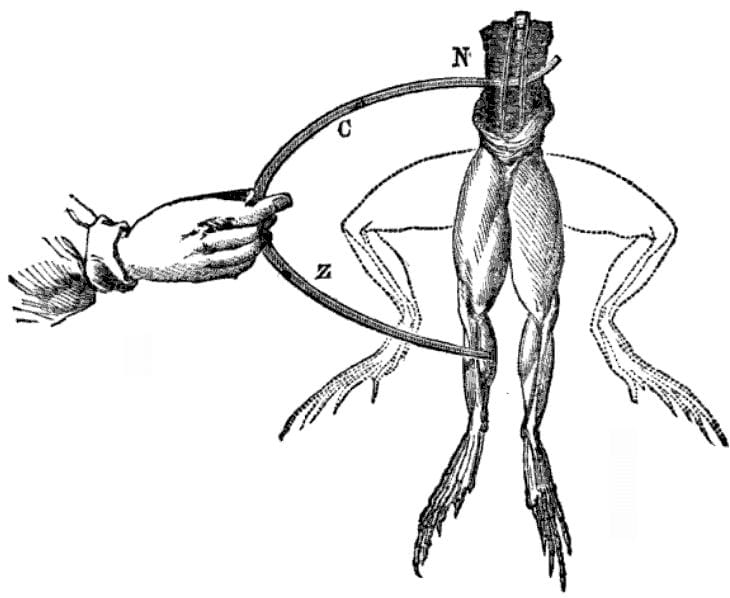
If you’ve read Frankenstein, you know that the discovery that there are electrical currents that controlled the expansion and contraction of muscles, including the heart, can be traced at least to the work of Luigi Galvini in the late eighteenth century. Electrocardiography is a much more recent development — in 1887, August Waller recorded the electrical activity of the human heart using a mercury capillary electrometer. In 1901 Willem Einthoven, generally credited as the “father” of the ECG, used a string galvanometer to record the beating heart — work for which he was later awarded the Nobel Prize.
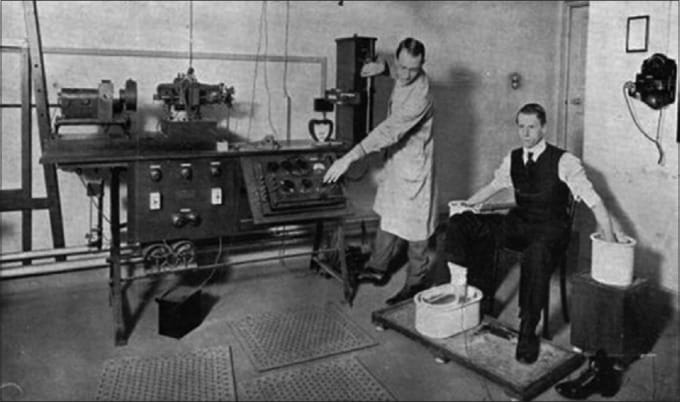
Obviously these early machines were very large and for quite some time required the patient be stationery to take their measurements — not conducive to testing to see if your easy run is really in “Zone 2.”
Of course, that didn’t stop Robert Bruce, who in 1963 devised the Bruce Protocol, better known as the cardiac stress test, which has a patient, with electrodes attached to their chest to monitor their heart, walk on a treadmill. Every 3 minutes both the speed and the incline of the treadmill are increased. The patient’s breathing and circulatory functions were analyzed for signs of potential problems.

The development of more portable devices came with the Holter Heart Monitor, which was released commercially in the early 1960s. The Holter machine was designed to monitor patients who had histories of occasional arrhythmias — it could be worn during regular daily activity, rather than requiring the patient to lie still for the duration of a test. (The original prototype weighed 85 pounds, but its size was eventually brought down to “less than cigarette package size to be worn inside a man’s jacket handkerchief pocket.”)
Although the editors of WIRED want you to believe that the history of technology is a history of scientific innovation alone — “what technology wants,” as Kevin Kelly once put it — cultural context always matters. Work on heart-monitoring machinery, alongside advances in heart medicine more generally, came in response to a rapid uptick in heart disease in the 20th century — work that continues today culturally and scientifically. Indeed, despite making progress in the detection of cardiovascular disease and in the prevention of cardiovascular mortality, heart disease remains the leading cause of death, responsible for about a third of all deaths globally. Thus, the prevalence of heart disease can make the kind of technological surveillance promised by fitness trackers an imperative — of course you’d want to track your heart-rate, even if, like Gilgamesh, many of us have only the most superficial understanding of what a pulse might indicate other than “alive” or “dead.”
Taking advantage, arguably, of our lack of medical expertise, fitness watches encourage us to turn over our training to the heart-rate monitor. It’s been this way since 1977, when Seppo Säynäjäkangas invented a battery-operated monitor to aid the training of the Finnish National Cross Country Ski Team. Säynäjäkangas went on to found the company Polar Electro, which released the first wireless heart-rate monitor in 1982. The device transmitted heart-rate data to a watch so that athletes — endurance athletes, primarily — could track the intensity of their workouts. (I mean, they could track them before, of course, using something like “Rate of Perceived Effort.” But data! “Real-time data!”) According to Finnish triathlete Pauli Kiuri, “At some point during your run, you get the feeling that you can’t push any further. But if your rate is still only 160 bpm, you just have to believe that yes, you can!”
Soon, athletes were encouraged to wear their heart-rate monitors not just during training, but all day long. Again, as with the ancients, the heart was seen as the window into health. By analyzing one’s heart-rate during exertion and at rest and upon waking, one could fine-tune one’s training, ramping up or dialing back the load according to how the heart responds.
Or so the argument goes.
Despite the accuracy with which these devices can measure our heart rate, where things sort of fall apart is the devices’ analysis of this number. That is, what should be heart rate be? What should it be when I’m running? Is it too high? Am I dying? You know, those sorts of things.
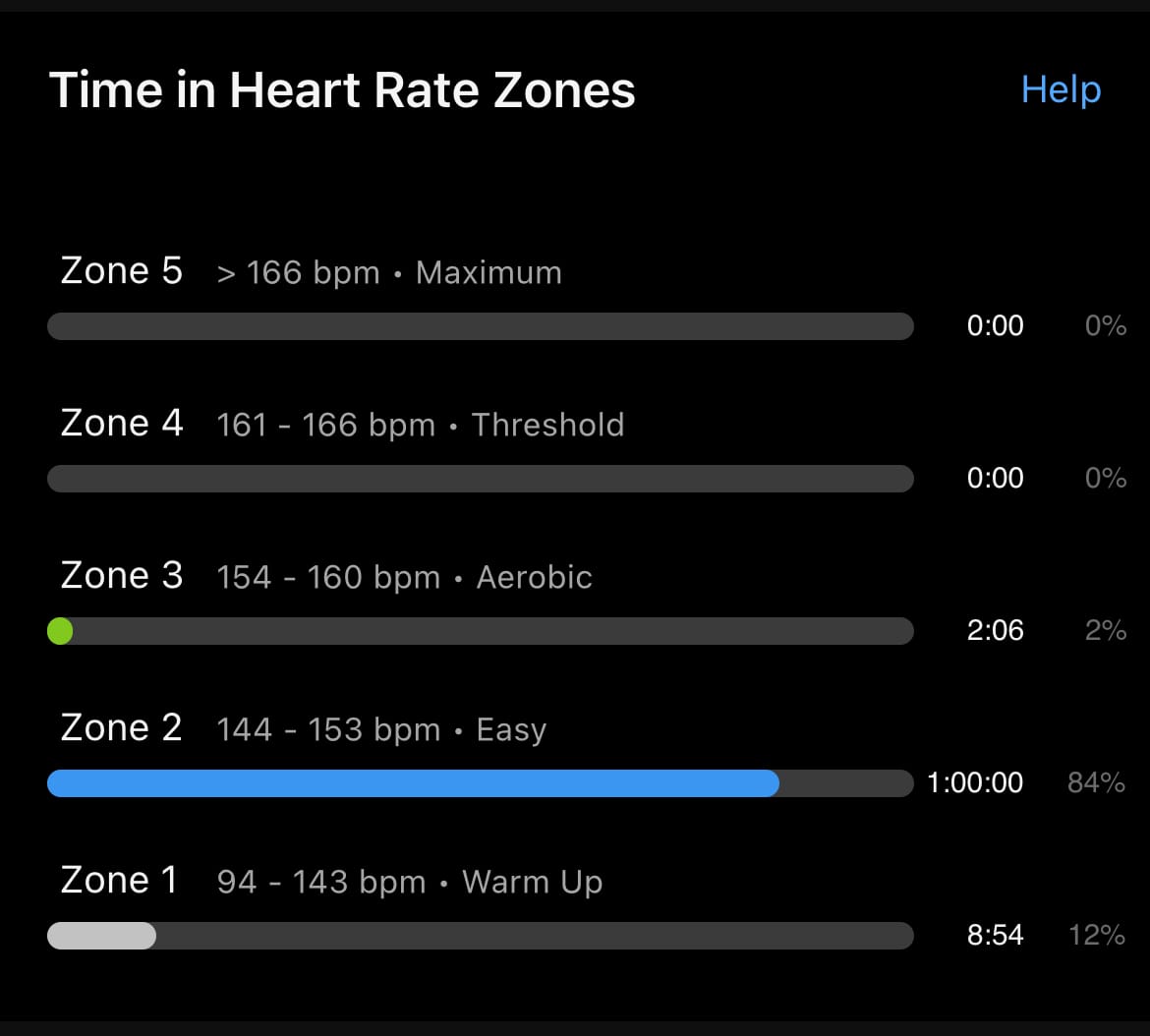
Along with the development in the 1980s of the heart rate monitors for athletes came a number of physiological insights and from there, training prescriptions. Typically, when one’s watch tells you what your average heart rate was during an activity, it will also tell you what “zone” it was in. My Garmin lists 5 — Zone 1 is 60-70% of your maximum heart rate; Zone 2 is 70-80% of max heart rate (and this, according to many running coaches is where your heart rate should be during the majority of your runs); Zone 3 is 80-90%; Zone 4 is 90-100%; and Zone 5 is 100-110% of max heart rate. Wait a minute, right? How can your heart rate exceed your maximum heart rate — don’t words have meaning in sports science? And how does your watch even know your max heart rate?
Heart rates, we do know, vary based on age — your watch will likely estimate your maximum heart rate based on 220 minus your age. But this is just an estimate and is more than likely totally wrong. It’s not just wrong because you might be more or less fit than the formula accounts — although yes, that’ll certainly impact your cardiovascular health. It’s wrong because this formula — the Haskell & Fox formula — was “never supposed to be an absolute guide to rule people's training,” as Haskell told The New York Times in 2001. Indeed, he and Fox gathered the data for their formula from a dozen or so published studies on heart disease that had tested patients’ heart rates. So, not at all a representative sample of the population. And, testing your maximum heart rate in a cardiologist’s office involves that classic “stress test” on the treadmill, where untrained individuals may well tap out of the test because their knees hurt, not just because their lungs do.
Nevertheless the Haskell & Fox formula has been widely adopted in the field of sports science (although, in fairness, not without some criticism). It was used in the software that accompanied the first commercially available Polar heart rate monitor. And it’s now hard-coded into our fitness watches. For all the talk of personalization, precision, and innovation, we’re wearing devices that might signal something else entirely.